Consent and authorisation
Clinical guidance around gaining consent and authorisation from a donor family
Increasing consent and authorisation rates
Opinion polls suggest that as many as 90% of the UK population support donation and transplantation but the family consent and authorisation rate hovers around 65%. This shortfall perhaps reflects the difference between what an individual might wish to happen after their death and the reality that faces a grieving family.
An increase in consent/authorisation rates to 85% would deliver almost 500 additional donors annually, and as a result is widely regarded as the element of the donation pathway most in need of improvement. It is also an element that for most parts of the UK has hitherto proven stubbornly resistant to change.
Family decline rates are the biggest single identified obstacle to organ donation in the UK. Interventions to reduce decline rates should continue to be a priority for all donation committees and collaboratives.
There are three broad and complementary strategies to increasing consent/authorisation for organ donation – ensuring a planned and collaborative approach in the way donation is raised with a family, promotional behaviour change campaigns that seek to improve the public's support for donation and legislative reform that might 'reset' societal expectations.
Wales introduced a system of 'deemed consent' for organ donation in December 2015, Jersey in July 2019, England in May 2020, Scotland (deemed authorisation) in March 2021 and Guernsey in January 2023. Northern Ireland plan to introduce their deemed consent law on 1 June 2023. The Isle of Man plan to introduce a similar law but have not confirmed a date to implement.
| Nation | Deceased Organ Donors (per million population) | DBD Consent / Authorisation Rate (%) | DCD Consent / Authorisation Rate (%) | Overall Combined Consent / Authorisation Rate (%) |
|---|---|---|---|---|
| England | 23.5 | 72.3 | 65.2 | 68.3 |
| Northern Ireland | 26.1 | 65.4 | 62.5 | 64 |
| Scotland | 18.4 | 74.8 | 55.2 | 64.8 |
| Wales | 27.1 | 74.6 | 66.7 | 70.7 |
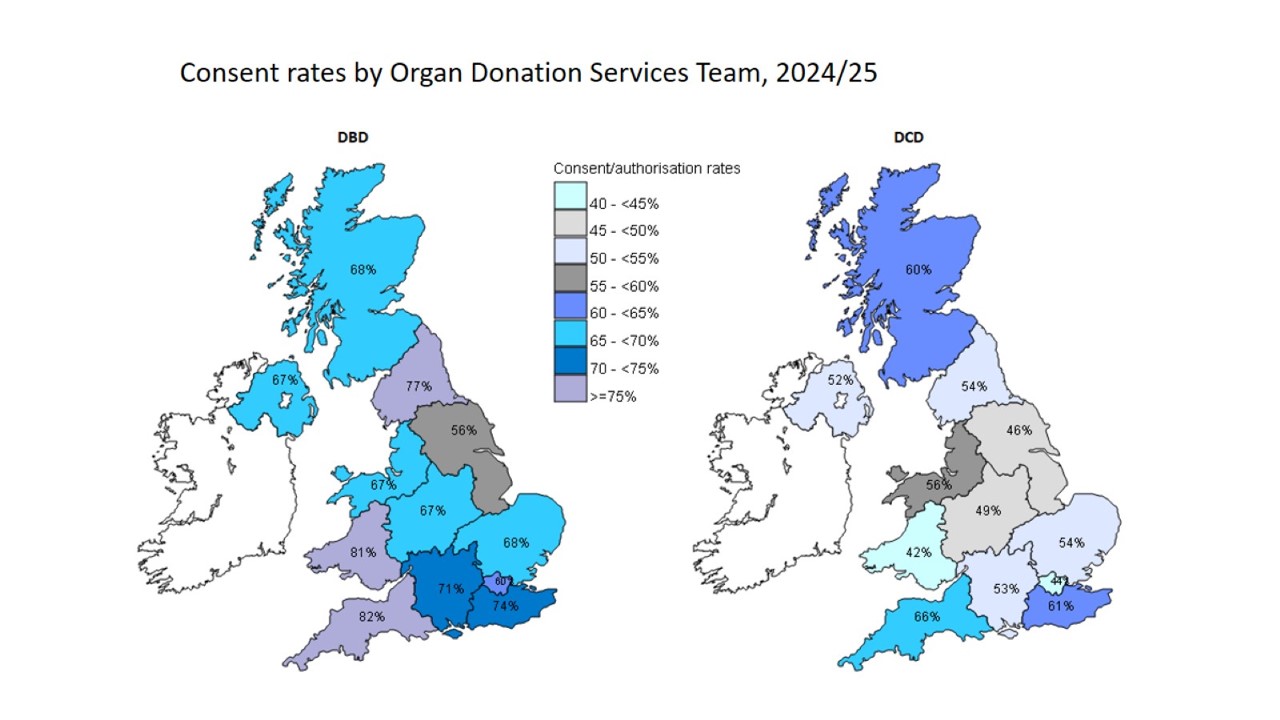
An organ donation services teams comparison
There are twelve regional teams covering the 4 UK nations and supporting the promotion and delivery of deceased organ donation activity in every hospital they cover. The diagram below illustrates the UK consent/authorisation rates for donation after brain-stem death (DBD) and donation after circulatory death (DCD) by organ donation services teams.
Disparities in consent/authorisation rates are multifaceted, and based on population demographics, numbers and types of hospitals (e.g. regional neuro-surgical centres), legislation and much more besides.
Family refusal rates are the biggest single identified obstacle to organ donation in the UK. Interventions to reduce refusal rates should be a priority for all donation committees and collaboratives. If the introduction of an opt-out system into Wales proves successful, it is possible that similar frameworks may be adopted elsewhere in the United Kingdom.
NHS Blood and Transplant (NHSBT) best practice
The following best practice and resources are relevant for approaching families throughout the UK. As per the Guidelines for the Provisions of Intensive Care Services, Edition 2 (GPICS2): “The consultant leads on breaking bad news before handing over to the [specialist nurse] when it is clear that the family have accepted the inevitability of their loss AND are ready to consider what may happen next.”
The family approach is considered in three stages. The specialist nurse / specialist requestor should be involved in all stages.
The language used in the following videos reflects that used in England. Each country or territory will use different wording based on their individual legislations e.g. authorisation is used in Scotland rather than consent.
Planning
It is important that there is agreement in advance on who will cover each element of the process and where the transition in responsibility will be.
An ideal example of effective planning is shown in this video.
Breaking bad news
In NHSBT we have developed a suggested model for breaking bad news and introducing the donation conversation which is loosely based upon a ‘Shakespearian tragedy’ by adopting a prologue and 3 act structure. The model provides a defined framework for the conversation, incorporating checkpoints along the way to ensure the family accepts the inevitability of their loss AND are ready to consider what may happen next. Only then are the family likely to be in a position to begin contemplating organ donation. Though all families are different which emphasises the important point of having a specialist nurse present for all stages.
Using this structured approach, the Consultant leads on breaking bad news (prologue, Act I & Act II) and then, after a break (interval), the specialist nurse will take the lead when it is clear that the family have accepted the inevitability of their loss and are ready to consider what may happen next (Act III). The transition to the specialist nurse should be delayed if it is clear that the family has not come to terms with the inevitability of their loss.
Approaching for donation
The specialist nurse will have checked the organ donor register which will inform how this conversation starts. This will need to be explored with the potential donors’ family to understand if this was their last known decision.
In this conversation the SNOD will explain to the family the benefits of donation, inform them of any check on the organ donor register, explain the full process and answer any questions, and support with any faith or belief requests.
Consent / Authorisation is governed by the appropriate acts for each nation (see resources section).
Deemed consent legislation (England, Wales, Jersey, Guernsey and Northern Ireland from 1 June 2023)
In England, Wales, Jersey and Guernsey deemed consent legislation has been implemented. Northern Ireland plan to introduce this 1 June 2023. This means that if you are not in an excluded group, and have not confirmed whether you want to be an organ donor - either by recording a decision on the NHS Organ Donor Register , or by speaking to friends and family – it will be considered that you agree to donate your organs when you die.
The following videos and presentations have been made by NHSBT to support clinicians operating under a deemed consent legislation framework.
Deemed consent in England: What clinical staff need to know
Talk by Dr Dale Gardiner (National Clinical Lead for Organ Donation). For use in hospitals.
Human Tissue Authority Codes of Practice (England)
Talk by Cathy Miller (Project Lead: Legislation Change Programme)
The Coronial Gift of Life
This video provides information to HM Coroners in England about how their role impacts on the outcome of organ donation. Also applicable to Coroner’s Officers, Deputies, Police, Pathologists and Mortuary workers.
Deemed consent in England: Approaching families, a clinical guide
Talk by Dr Dale Gardiner (National Clinical Lead for Organ Donation).
Family approach and deemed consent example scenarios
The following videos show examples of the family approach and deemed consent scenarios in England. These links will open in a new window.
Planning meeting
The meeting to plan how organ donation will be discussed with family members is crucial to ensure the end of life discussions are clear and well delivered.
Scenario 1: the deemed conversation
This video provides an example of how to introduce deemed consent during the organ donation conversation.
Scenario 2: never heard of it
Although there was a large scale marketing campaign about Max and Keira’s law, there will be some families who do not know about it. This video provides and example of how to discuss deemed consent in this scenario.
Scenario 3: Known decision
A known decision represents an opt in or opt out by the potential donor. Here we see how address this conversation when the patient has already made their decision known to those close to them.
Opt out
An opt out on the Organ Donor Register must still be communicated to the family so they’re aware of why donation cannot go ahead.
ODR Status change
There have been occasions where the family register a donation decision on behalf of the patient while they are in hospital (and incapacitated). This video provides an example of how to sensitively approach this.
Nominated Representative
A nominated representative sits highest in the hierarchy of qualifying relationships but it is rare to encounter one. This video illustrates how to bring in the nominated representative while still involving the family in discussions.
Family raise donation
It is not uncommon for the family to raise the subject of donation. This video provides an example of how to navigate that conversation.
Organ donation websites
Wales
Visit the Welsh government website (English version)
Northern Ireland
Visit the Organ Donation Northern Ireland website
Scotland
Visit the Organ Donation Scotland website
Jersey
Visit the Jersey Government website
Legislation and Codes of Practice
Wales
- The Human Transplantation (Wales) Act 2013
- Human Tissue Authority Codes of Practice for Wales (updated May 2020)
Jersey
England
- Organ Donation (Deemed Consent) Act 2019
- Human Tissue Authority Codes of Practice for England and Northern Ireland (PDF 941KB)
Scotland
Guernsey
National Institute for Health and Care Excellence (NICE) clinical guidance
In December 2011, the National Institute for Health and Clinical Excellence (NICE) published a short clinical guideline on organ donation (CG135). This guideline, which applies to practice in England, Wales and Northern Ireland only, includes detailed recommendations on how to best approach the family of a potential organ donor. Key messages from this guidance are that:
- the family approach should always be planned in collaboration with the SN-OD
- the approach should only occur when it is clear that the family have accepted the inevitability of their loss
- apologetic and negative language should be avoided and instead that donation should be presented a positive act that is part of the care that a dying person might wish to receive
- the individual leading the family approach must be competent to do so, have the requisite knowledge to answer any family questions and have the time to take the family through what can be a lengthy process.
November 2015 - NICE has published interventional procedure guidance on living-donor liver transplantation IPG535.