International perspectives
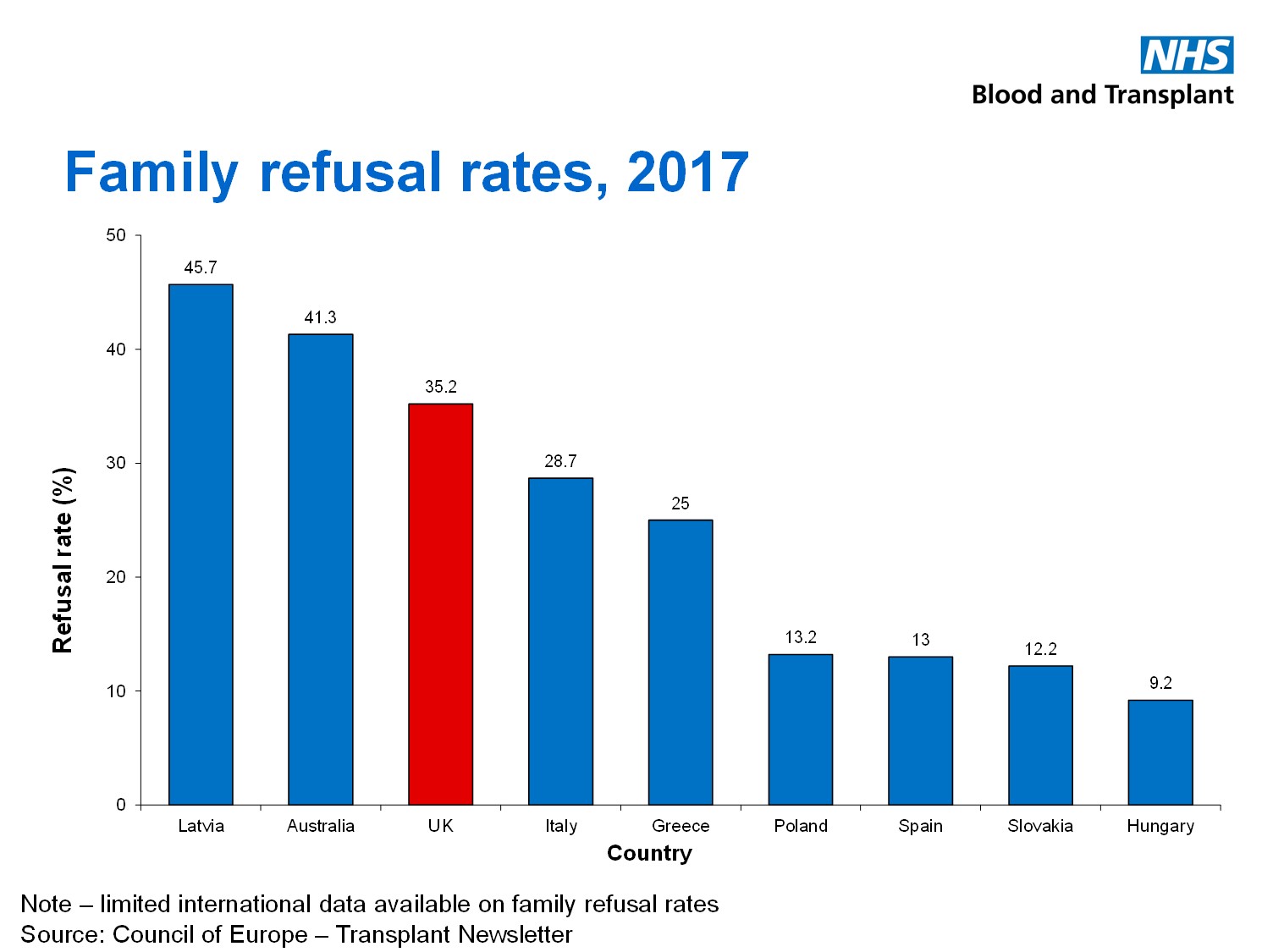
Family refusal rates in the UK are considerably higher than those reported from many parts of mainland Europe, where they are often less that 20%.
How can family consent authorisation rates be improved? It is tempting to believe that the solution lies exclusively with public promotion and societal engagement. However there is also evidence that the way in which the possibility of donation is presented to a grieving family can have a critical impact – both positive and negative - upon the decision that they make. It is particularly important that families are approached at the appropriate time, in the appropriate fashion and by someone with the appropriate skills.
It is not always appreciated how difficult such decision-making can be for many families at this time and how seemingly innocuous remarks can lead to a family closing the door on the donation discussion. If families are to be given the best opportunity to make the decision that is right for them, specific factors need to be considered, identified and planned for by health care professionals who are both knowledgeable and experienced.
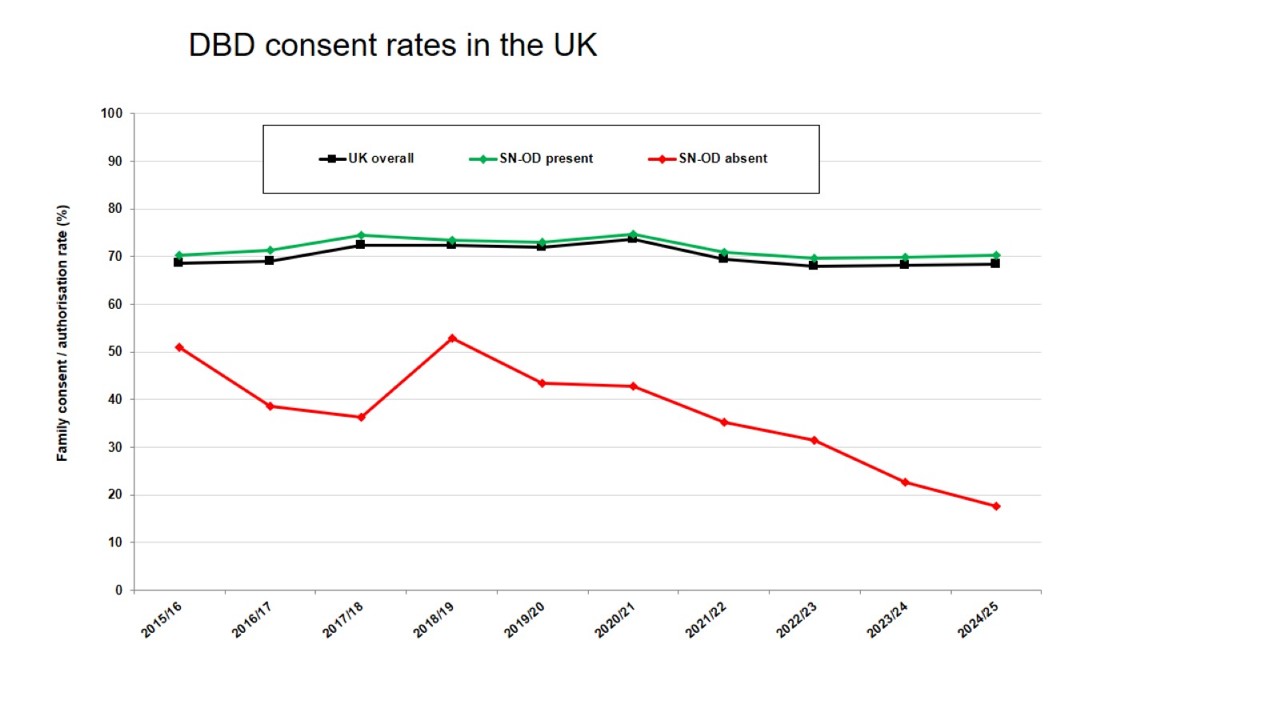
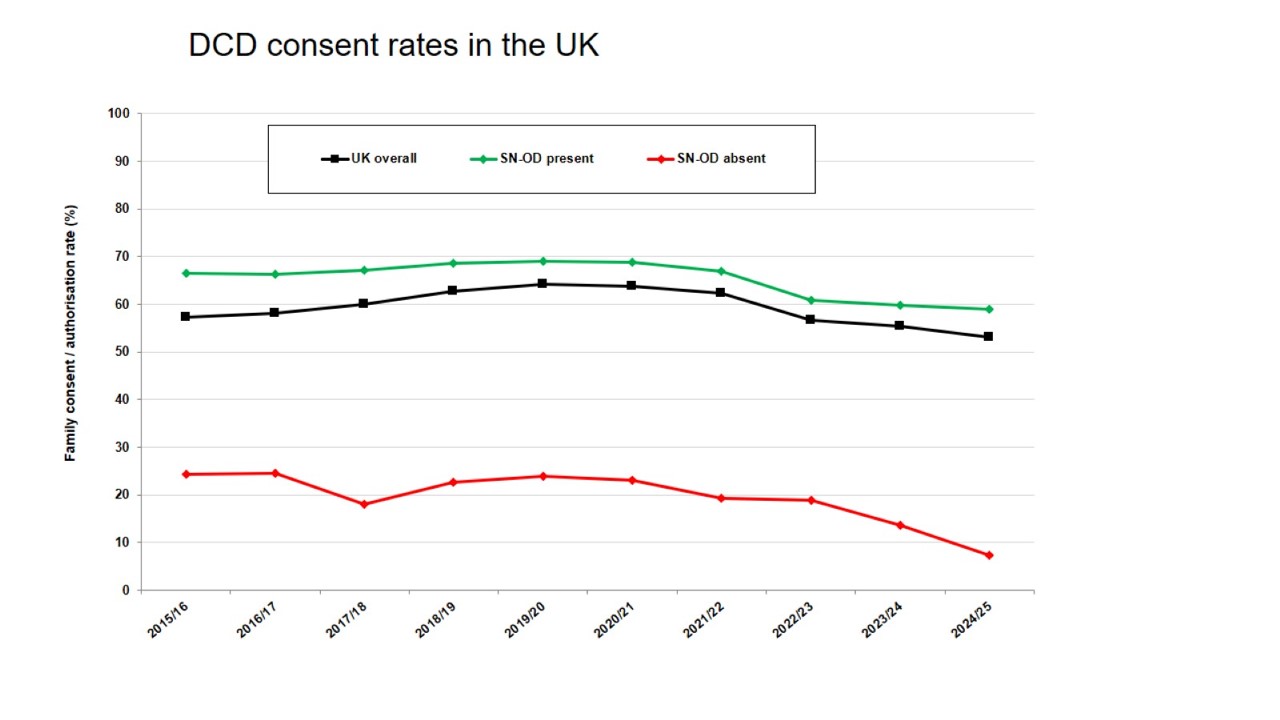
Furthermore, whilst donation will always be a relatively infrequent activity for the majority of critical care clinicians, it is the core activity of Specialist Nurses in Organ Donation (SN-ODs). International evidence would suggest that co-ordinator led approaches achieve higher consent/authorisation rates. Although the ACRE study failed to replicate this finding in UK practice, it did not in any way evaluate best practice as currently described. Furthermore, audit data from NHS Blood and Transplant repeatedly reveals higher family consent / authorisation rates for both DBD and DCD when SN-ODs are involved at an early stage (see Figures 2 and 3).