Medical Director Bulletin
Monthly communication from the ODT Medical Director
Organ and Tissue Donation and Transplantation Directorate January/February 2025
A message from Professor Derek Manas, Medical Director OTDT:

Hello again from me and the clinical team.
I’d like to start by welcoming Carla Rosser. Carla has been appointed to a joint CCS post with Southmead which will be 3 days based in Southmead as the new H&I CCS Head of Laboratory to support their Renal Transplant Programme, and 2 days with NHS Blood and Transplant (NHSBT) primarily as the new OTDT H&I lead.
I would also like to officially welcome Chris Johnston from Edinburgh, who has been appointed as the Deputy Chair of the Retrieval Advisory Group (RAG). We look forward to working with both of you.
Just a reminder that this year’s British Transplant Society (BTS) and NHSBT's Joint Congress starts on the 12 March 2025 and I hope to catch up with many of you in Brighton.
The Headlines
SCORE
The Sustainability and Certainty in Organ Retrieval programme once again continues to progress its work. As mentioned before, the 'workforce' work-stream have produced their recommendations and you should have received email correspondence about establishing retrieval collaboratives, which I hope is progressing well. The transport work-stream led by Mark Roberts have completed their deliberations and we'll await the final recommendations sign-off.
Histopathology
Implementation decisions on the national plan business case is still awaited from NHS England (NHSE), but the interim plan has unfortunately hit a roadblock due to a process issue. Suffice to say this is extremely disappointing, especially for the working group that have put a huge amount of time and effort into this, but we have appealed the decision and await a response from NHSE.
Living Donor Liver Transplantation (LDLT)
Once again, I am pleased to report that there has been ongoing engagement with the Proctor MDT and potential pairs continue to be referred in for consideration, and the next transplant may be soon in the offing. I'd like to congratulate the BTS executive for organising a fantastic meeting in London held at the end of last year, in collaboration with the international Living Donor Liver Transplant Society.
We (OTDT) presented our LDLT Proctor Program and were highly commended. Just as a reminder, the website has all the information centres need to engage the proctor team and there is educational resource for clinicians and patients as well as a link to patient educational films available (See Lisa's update further on in the bulletin).
Cardiothoracic Review
The NHSE Transformation programme for Cardiothoracic Transplant Services led by Maggie Kemner and Simon Kendal is now underway, and OTDT are stakeholders in the work. Currently there are a number of engagement meetings and workshops going ahead to scope out what’s needed to cover the remit.
Mr Marius Berman from Papworth and Dr Anna Reed from Harefield are the subject matter experts and I will ask them to give an update from their perspective in a few months' time, but there is a short update from Laura Barton further on in this bulletin.
ISOU
A Commissioning Symposium went ahead on the 6 November 2024 and was very well received. There is now a recent report highlighting the importance of strengthening collaboration between NHSE and NHSBT, ensuring the patient voice is heard, understanding the new commissioning structure and processes within NHSE and developing the Transplant Oversight Group (TOG) which is a committee in parallel between the two organisations chaired by Matt Day and Anthony Clarkson.
The Trust Engagement Sub-Group chaired by Chris Callaghan and Mark Cubbon, focusing on OUG Recommendation 10 are close to completing their work and will soon submit the recommendations in the form of two documents, one advising Trusts/Boards on the requirements expected of local trust Organ Utilisation committees and the other focussing on what to monitor.
The Genomics Subgroup chaired by Rommel Ravanan and Richard Battle, the Xenotransplantation Subgroup chaired by John Iredale and Anthony Clarkson and the ARC subgroup chaired by John Casey and Shamik Gosh have all submitted their recommendations.
Organ Utilisation Group Implementation
Recommendation 3 - CLUs
- Local CLU survey action plan to be progressed, and local CLU focus group to be diarised
- Focus on CLU KPIs and Measures of Success – proposal ready for OUG-RIO in Jan.
- Lead Heart CLU role to be advertised
- Development of standardised Terms of Reference / guidelines for unit decline meetings in development shared – in consultation, for launch in early 2025, and tabled for next OUG-RIO meeting
- Offer Review Scheme - trend analysis to be developed and assessed.
- 2025 Comms Plan to be launched
Organ Utilisation continues to hold up well, and this will be due to a combination of the impact of CLUs on culture change and use of machine perfusion technology. Some possible metrics are being developed.
Recommendation 4 - Transplant collaboratives
Continue to progress establishment of the transplant collaboratives, focusing on liver. The renal collaboratives 8-point action plan has been developed post national meeting, for rollout, with areas of focus to include:
- The development of local collaborative 25/26 workplans,
- Paediatrics Collaboratives Plan Development and;
- Engagement with Commissioners
Recommendation 8 - ARCs
ARCs next steps to include service specification development, industry collaboration development, commissioning option appraisal, target operating model test framework (livers), pre-recruitment preparation, and comms/socialisation plan.
Recommendation 9 - National Oversight System for Innovation in Perfusion and Preservation
Survey responses being reviewed to improve quality of data, and to be shared at OUG-RIO at end of January 2025.
Recommendation 10 - Define national measurable outcomes to monitor and evaluate success
PREMS/PROMS group to meet alternate months going forward, to maintain progress for solid organs PREMS/PROMS and DREMS/DROMS.
Kidney, Heart & Lung PREMs in development (pre-tested PREM due Summer 2025) [Clinical Research Fellow & BTRU) [Liver PREM developed and plan for launch to be identified]
Other Organ Utilisation-Related Activity
- Economic Benefit of Transplantation: Short term plan in progress, with RTC workshops to collate waitlist / counterfactual data planned for January
- Economic Sustainability in Transplantation: Strategy and workplan in development, and 2025 Comms Plan to be launched
- CT Review - Scoping meeting expected February 2024
- Development of Islet Transformation workplan, following December Islet Summit
Await update from NHSE regarding renal service spec, to be effective from 1 April 2025
ERAS, Clinical Collaborative, Sustainability Agenda
The Early Recovery after Surgery for transplant patients (ERASTx) continues to progress well. (Please see the update from Lisa further on in the bulletin)
A National Kidney Collaborative Engagement meeting held on the 9 December 2024 in London was very successful and output from the meeting are being progressed. The Liver and CT collaboratives are in progress. Thank you to Gareth Jones, Laura Barton and Abby Horne for all their hard work on this.
The OTDT Environmental Sustainability Working Group led by Matt Welberry-Smith continues to provide the transplant community with resources to help reduce the environmental impact of transplant activity. Matt has provided an update further on in the bulletin.
BTS Monothematic Meetings
On the 7 November, British Transplantation Society held a meeting on aging in transplantation and on the 8 November they hosted members of the the international living Donor liver transplant society to discuss the current state of living liver donation.
Adult to Adult Living Donor Liver Transplant Proctor Program
This program went live in mid-July and we have had 8 pairs referred into the proctor team. They have successfully proctored their first transplant at the Royal Free Hospital on the 29 October.
I would like to congratulate the team for their commitment to this project and thank Lisa Burnapp for her leadership. Again, I would urge you to look at the website and review the excellent information and educational recourses that are available.
iOrbit Project
The lack of corneal tissue still remains a priority for NHSBT, and the iOrbit project will be updated in the next bulletin.
Consent
Consent to Organ Donation remains low at 59% and there are now several initiatives on several fronts. A Consent Summit is planned for April this year in conjunction with DHSC. There are a number of marketing initiatives now implemented.
Islet Summit
On the 10 December 2024, we held an Islet Summit in London to look at future proofing the national Islet isolation service. The report from that meeting is available and a working group has been established to progress the recommendations.
Yours sincerely,
Professor Derek Manas
Medical Director – OTDT
NHS Blood Transplant
Obituary, in memory of Prof. Dr. Frans Claas
Message from Matt Welberry-Smith, Chair of the Envronmental Sustainability in Transplantation (ESIT) Group:
The climate emergency faces all health services with the need to adopt the most sustainable practices available. All NHS services can contribute towards reaching environmental targets and reducing our collective impact. With our high levels of activity, the transplant community has significant potential these environmental impacts, and to contribute to environmentally sustainable clinical practise.
Join us online for the exciting official ESIT launch and learn about:
- ESIT's key focuses for the year and our long-term strategy
- Real world examples of positive green change in clinical services
- How you can become an environmental champion in your Unit and what help we can offer
- Share your ideas about how to make NHS transplant services greener
Don't miss this opportunity to be part of the community and help make transplantation environmentally sustainable. Register now and be a part of the change!

Key details
The online launch starts on Tuesday 1 April 2025, 1pm to 2pm.
Message from Ian Currie, Associate Medical Director for Retrieval:
Key Diary Dates:
2025 and 2026 dates will be released shortly.
These will be November 2025 for the Virtual masterclass and January 2026 for the Cadaveric Masterclass.
National Organ Retrieval Services Virtual Masterclass
The National Organ Retrieval Services (NORS) Virtual Masterclass was held in November 2024 and broadcast live from York.
This comprehensive 3-day programme was open to all UK and International delegates. We had over 120 delegates joining each day and had registrations from Jerusalem, Israel, Dublin, the Netherlands, Nepal, New Zealand, Guernsey, India, Spain and not forgetting all those joining us from across the United Kingdom.
This was a great achievement, sharing our expertise worldwide, and it was great to have such a diverse and far-reaching audience. This course has a complex technical set up and we welcomed the support of an audio-visual team from Tapestry for the 3 days.

Day one, open to all NHSBT staff with an interest in organ donation, retrieval, and transplantation, was well attended and we received great feedback on their experience of this course. Here are some quotes from our evaluations:
We were also delighted to welcome and be joined by other healthcare professionals with a keen interest in organ donation, organ retrieval and organ preservation including perioperative practitioners, perfusion specialists, Specialist Nurses-Organ Donation and Clinical Leads in Organ Donation (CLODs).
One international delegate commented "This course has provided me insightful learning of how intricate the process of organ donation here in the UK. I will further develop my effective communication skills as it was emphasise how relevant it is during retrieval"
Here are some more testimonies and quotes from our evaluations:
Meet some of our faculty, organisers and observers who joined us on site in York:

Left to Right (from the bottom).
Marius Berman, NHSBT & Papworth, Ian Currie, NHSBT & Edinburgh – Course Directors
Fiona Hunt; Edinburgh & NHSBT and Cecelia McIntyre, Newcastle & NHSBT
Lynsey Farwell, Edinburgh and Sarah Beale NHSBT
Chris Johnson, Edinburgh and Pradeep Kaul, Papworth
Shahid Farid, Leeds and Jennifer Baxter, Papworth
Helen McManus, NHSBT and Cathy Miller, NHSBT
Gordon Turpie, NHSBT and Olive McGowan – Chief Nurse, NHSBT
UK National Organ Retrieval Services Cadaveric Masterclass
The UK National Organ Retrieval Cadaveric Masterclass (CMC) course is for UK surgeons seeking full registration with NHS Blood and Transplant to lead their NORS team and perioperative practitioners involved in organ retrieval and preservation.
This year's course was held at the state-of-the-art Cambridge Surgical Training Centre and was a great success. Below is a photo of all the faculty and delegates from across the UK. We were once again supported by the audio-visual team from Tapestry who provided excellent live high resolution video footage throughout the 2 days, of which the quality was fantastic.

We were also joined by our Chief Nurse – Olive McGowan who commented this about the course:
"Sometimes we attend courses and conferences and they are good, but I'm here at the CMC and all I can say is it's totally out of this world."
Here are some evaluation quotes from the delegates:
"Excellent facilities, very enthusiastic and knowledgeable faculty" and;
"Excellent teaching and live demonstration, I really got hold of the steps involved in retrieval after this course."
News
We will shortly be opening a LearnPro channel exclusively for all UK NORS retrieval team staff, whether or not your trust has a LearnPro contract.
This will feature a video library, which will eventually cover all aspects of nursing and surgical education in Retrieval. For staff to access this resource, we need NHS email logins for all NORS staff - contact the perioperative lead or NORS lead in your centre.
For any other further details contact Professional.DevelopmentODT@nhsbt.nhs.uk or check out UK Organ Retrieval Masterclass - ODT Clinical - NHS Blood and Transplant
Message from the Organ Utilisation Development Team & Clinical Leads for Utilisation Teams:
Organ Utilisation Development Team and Clinical Leads for Utilisation:
In the last bulletin we confirmed that Diana Garcia Saez, National Clinical Lead for Cardiothoracic Organ Utilisation since 2020, and Aaron Ranasinghe, Lead Heart CLU since 2021, have both stepped down from the CLU roles. We are very grateful for the excellent work and significant contributions that Diana and Aaron have both made. As a result of these changes, Vicky Gerovasili has stepped into the role of interim National Clinical Lead for Cardiothoracic Organ Utilisation as well as continuing as Lead Lung CLU. Nick Inston will be interim National Clinical Lead for Abdominal Organ Utilisation as well as continuing as Lead Kidney CLU. Thank you to Vicky and Nick for taking on these dual roles. The post of Lead Heart CLU has been advertised, and interviews are due to take place shortly.
We have a busy year planned for 2025 within the Organ Utilisation Development Team and Clinical Leads for Utilisation (CLU) community. Some of our priorities for the year ahead include:
- Elevating the profiles of the Clinical Leads for Utilisation at a local and national level and extending our engagement to the wider MDT.
- Rollout of a standardised organ decline meeting framework.
- Development of an Organ Utilisation Education Strategy.
- Focus on increasing patient engagement within organ utilisation.
- Planning for our annual National Organ Utilisation Conference (NOUC).
We have also launched our 2025 CLU Learning Series, which starts on 9 April as per the flier below – we’d love for you to join us, so please register for your place now.
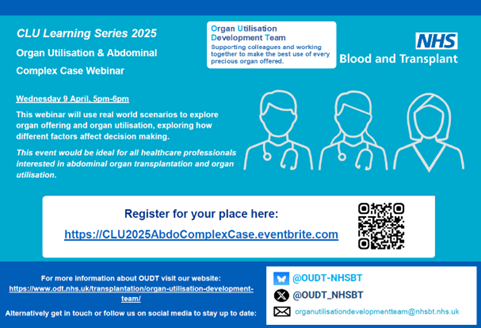
Key event details
Event name: Organ utilisation and abdominal complex case webinar
Event date: Wednesday 9 April, 5pm to 6pm
Register your place on eventbrite
Find out more about the Organ Utilisation and Development Team
Watch out for further dates to be announced later in the year, by following us on social media, or by getting in touch.
With best wishes.
The Organ Utilisation Development Team - Chris Callaghan, Nick Inston, Vicky Gerovasili, Liz Armstrong, Carrie Scuffell and Laura Barton
Message from Olive McGowan,Chief Nurse, OTDT Patient Safety Team:
Dear Colleagues,
Two messages from the Patient Safety Team:
Please find attached to the bulletin a report that provides detail on: Events investigated for possible donor-derived transmission of infections, malignancies, and other cases of interest. April 2023 - March 2024.
Thank you to everyone for reporting and assisting us to investigate all incidents and concerns reported.
HHV8 Infection:
I would like to inform you that the HHV8 documents are now on the website, and this includes a new document: NHSBT/BTS Joint Consensus Document for Management of Human Herpes Virus 8 (HHV-8) in Solid Organ Transplantation (SOT).
https://www.odt.nhs.uk/transplantation/tools-policies-and-guidance/policies-and-guidance/
Can I remind you that the following cases need to be reported to OTDT so we can keep track of the numbers, monitor the recipients and their outcomes. As ever, we need to inform all centres and colleagues of any positive of indeterminate results. They are also reportable to the HTA.
Please report any of the following new:
- Confirmed new infection in a SOT recipient (confirmed PCR positivity) , regardless of known donor HHV-8 status; this includes patients who are being monitored for infection because they have received an organ from a donor who tested positive for HHV-8 at screening, or a patient who was tested for another reason and found to be positive.
- Patients who have been diagnosed with HHV-8 infection and have developed symptomatic disease, regardless of donor status (for example, it could be a case of a transplant that pre-dated the introduction of donor screening, or a patient linked to a donor who tested negative for HHV-8 at screening). It is the significant infection or disease that triggers the need to formally notify, after the initial email or telephone conversations about the case.
Many thanks,
Olive McGowan
Message from Colin Wilson:
OrQA-UK Trial
The Organ Quality Assessment team which includes NHSBT, academics from Newcastle and Bradford University, Quality in Organ Donation (QUOD) have secured to run a trial of an AI powered photograph analysis device to reduce the number of deceased donor livers not utilised.
The trial will be the first use of an AI tool in world transplantation. The aim is to reduce the number of livers not transplanted because of fatty liver disease (steatosis). Liver photographs will be taken and uploaded in the standard way. Within the TransplantPath platform 50% of the donor sets will be randomised to having an OrQA score embedded with the photograph and 50% will not. The team will then be able to work out what effect the AI tool has made. A key element of the trial will be making sure all the liver transplant centres are informed and aware of their own past data on the use of the fatty livers. The Clinical Leads in Utilisation (CLU-liver) team will facilitate the dissemination of this information. The plan is for the trial to start in late 2025 after all the research governance and IT infrastructure are in place. From a donor assessment perspective this should be very “light touch” as the trial should not need any extra forms or direct patient family involvement, but this will be clarified with the Research Operational Framework Group and the Retrieval Advisory Group.
Currently the tool purely assesses the steatosis score and gives a digital score alongside the standard surgical assessment of “None”, “Mild”, “Moderate” or “Severe”. For various reasons human donor surgeons tend to overscore the fat content of the liver, whereas the AI will analyse the photograph objectively with the benefit of iPad digital cameras. Ultimately the tool will give a lot more information to ensure the right decisions are reached. Further tools for kidney and pancreas are at advance stages of development and future versions will give detailed readouts on other features of transplantability and long-term outcome in the recipient. The team anticipate the AI will also be useful for other research projects, audit, governance and education as well. More information will be provided in further newsletters and meetings on this exciting project which marks the beginning of the AI revolution in organ donation.
USA/UK Transplant Exchange
The challenge of making the best use of donated organs is not unique to the United Kingdom. The USA has similar issues but on a much larger scale and a far less integrated healthcare system. Colin Wilson, who leads the Blood Transplant Research Unit theme on “Organ Utilisation” has set up a quarterly online meeting with the Organ Procurement and Transplant Network (OPTN) team in the States to share ideas, best practice and research progress on initiatives and projects to tackle the common issues.
The next meeting on Wednesday 5 March 2025 at 3pm, will look at the hot topics of organ perfusion, ARCs and NRP with contributions from Ian Currie, Marius Berman and David Nasralla. The meeting starts at 3pm and utilises the WebEX platform. If you would like to join please email Abby Horne via the MD Office PA inbox (MDOfficePAs@nhsbt.nhs.uk) who will send back a link to register.
The US perspective is always slightly different and stimulating!
Message from Laura Barton, OTDT Programme Manager:
ISOU & OUG
The next ISOU meeting is on 26 February 2025 and will receive recommendations from the following subgroups:
- Trust Engagement Subgroup, focused on Trust-level Organ Utilisation strategies (chaired by Chris Callaghan and Mark Cubbon).
- Xeno-transplantation Subgroup, focused on legislation, regulation, research and ethics (chaired by John Iredale and Anthony Clarkson).
Recommendations from the ARCs subgroup and Histocompatibility & Immunogenetics subgroup were received and endorsed at the December 2024 ISOU meeting and are awaiting ministerial review. Further, a report from the Commissioning Symposium is due to be published by March 2025, following the event in November last year. The report will focus on the outputs from the event, including opportunities strengthening collaboration between NHSE and NHSBT.
The next steps for ISOU and focuses for 2025 will also be discussed at this meeting. In the meantime a significant amount of work continues within NHSBT regarding OUG implementation, for which an implementation roadmap is available here.
Islet Summit:
The Islet Summit took place on 10 December 2024 in London. At this meeting the transplant community recognised the significant dedication, skill and hard work of the isolation teams in the UK, and constructively discussed key areas of focus and opportunities for delivering sustainability to the service. An Islet Transformation Fixed Term Working Group will now be established, led by John Casey and Steve White, with first meeting to take place by mid-April. The group will focus on the key recommendations from the summit, which include:
- Funding and commissioning – refreshing the service specification, development of metric and commissioning dashboard, costing review and NHSE and NHS Scotland joint commissioning opportunities
- Modelling demand and capacity to futureproof services (including SIK activity)
- Ensure service continuity with changes in technology due in the next 18 months
- Review the referral pathway, as well as opportunities for pathway standardisation and equity of access across the country
- Develop a laboratory workforce model and joint education programme
CT Transformation Programme:
Following the publication of the government's CT Information Collation Exercise, NHS England has now initiated its Cardiothoracic Transformation Programme. This is being led by Maggie Kemmner, Head of Heart and Lung Transplant Transformation, and Subject Matter Specialists and Patient Representatives have been recruited. The improvement areas for the Programme will include:
- Access to transplantation
- Short and long-term outcomes
- Patient experience of transplantation
- Sustainability of transplantation services
This will include cross-cutting themes such as holistic care, as well as organ allocation, within which NHSBT has a key part to play. A joint meeting took place on 5 February, with NHSE and NHSBT representatives to explore the best approach to partnership working within this transformation programme, with a commitment to all that there is much needed action needed in order to support the cardiothoracic transplant community to deliver improvements. Further updates will follow as this transformation programme progresses.
Message from Lisa Burnapp, Associate Medical Director for Living Donation:
Living Donor Kidney Transplantation (LDKT):
- LDKT activity is strong year to date and the proportion of identified transplants in each UK Living Kidney Sharing Scheme (UKLKSS) matching run that proceed has increased. Given the capacity constraints in some centres, this is an achievement.
- Registration is open for the UK Living Kidney Donation (LKD) Network Meeting on Thursday 15 May 2025 at Wolverhampton Racecourse. Access first programme announcement here: https://www.odt.nhs.uk/living-donation/uk-living-kidney-donation-network/
- The collaborative work in 2024 between the UK LKD Network and The Centre for Sustainable Healthcare to examine the carbon footprint of the living kidney donor assessment pathway has won a further grant from the National Health Foundation to disseminate findings and support pathway improvements. This is a key area for quality improvement and there is a session dedicated to discussion at this year’s network meeting.
- The Euro-KEP project, which builds on the work of the previous European Network for Collaboration in Kidney Exchange Programmes (ENCKEP) and sponsored by the EU Commission for 3 years, met for the first time in January. The UK is represented by NHSBT (Lisa Burnapp and Matthew Robb) and University of Glasgow Department of Computing Science (David Manlove and his team). A fixed time working group looking at the feasibility of international collaboration between the UKLKSS and other countries has been established, Co-Chaired by Lisa Burnapp and Matthew Robb.
Living Donor Liver Transplantation (LDLT) Programme:
- The launch of the Proctor Team programme to support the expansion of adult-to-adult living donor liver transplantation has resulted in 12 donor referrals (for 8 recipients) across 4 transplant centres. There has been positive feedback from centres involved. The first proctored case post-launch went ahead at the Royal Free at the end of October 2024. Both donor and recipient are doing well. Many thanks to all our Proctor Team members and to transplant centres who have engaged with the programme, it is beginning to gather real momentum
- Information about the LDLT project and Proctor Team programme can be found here: https://www.odt.nhs.uk/living-donation/living-donor-liver-transplantation/
- Donor and recipient information here: https://www.organdonation.nhs.uk/become-a-living-donor/donating-part-of-your-liver/
- The next UK LDLT Network Meeting will be held on Tuesday 16 September 2025. First Programme Announcement to follow.
Enhanced Recovery After Surgery in Transplantation (ERAS in Tx.)
- This programme, designed to facilitate the roll-out of ERAS in Tx. in transplant centres across the UK so that transplant recipients and living donors are empowered to contribute to a more effective post-operative recovery, continues to expand.
- It has attracted interest from more organ groups - a pancreas workstream was established in November 2024 and a lung workstream is currently being set up.
- This year will see the publication of living kidney donor and adult liver transplant recipient packages to add to the existing adult kidney transplant recipient package, available here: https://www.odt.nhs.uk/transplantation/enhanced-recovery-after-surgery/
Messages from the ODTD Marketing & Campaigns Department New Paid Media Campaign:
Organ Donation Paid Media Campaign in England and Wales
10 February 2025 to 31 March 2025

The campaign utilises our successful existing creative of 'The best thing you’ll do today' across all platforms and will involve two channels: a paid media partnership and social media advertising. Partnering with the Bauer network and particularly their Greatest Hits Radio station (GHR) for a seven week period, will see well-known presenters endorsing organ donation, display advertising across Bauer media magazines and podcasts and, a first for us, enabling opt-in registrations through smart speakers.
Audience:
We will be targeting adults aged 50+ in England and Wales, identified as the biggest opportunity for increased registrations, leading to increased consent. Partnering with Greatest Hits Radio is a natural fit for this audience as is a community connection, a lifestyle interest area, and a trusted companion with whom they engage daily.
Campaign Approach:
- We will disrupt listeners daily routines to make them see organ donation is important and urgent.
- We will enable them to register their decision quickly and easily.
How will the campaign look on-air?
GHR is the most listened to commercial station in the UK with a dedicated following, who look to radio to provide the soundtrack to their day and provide recommendations on what the latest must haves and dos are. It provides local and regional news updates, interviews, and community features to ensure listeners stay informed and feel connected to everyone.
Through a seven week-long partnership with GHR, primetime radio presenters will drive listeners to confirm their decision to be an organ donor by highlighting it at unexpected times during sponsored slots. These popular presenters will record and share several audio messages around Organ Donation; making listeners feel it’s important, urgent and a priority to act and confirm their decision on the NHS Organ Donor Register. This will cause (positive) disruption within an environment the audience are well accustomed to as it will be surprising and unexpected but delivered by trusted voices. The campaign will run across the Greatest Hits Network, including Welsh language formats on stations in Wales.
What will happen off air?
Simultaneously over the seven week period, Organ Donation digital display advertising will appear across Bauer's wide range of digital magazines, encompassing titles including Closer, Puzzles, Yours, Country Walking, Gardening and Classics Cars Weekly, making registration as easy as the click of a button (through to our website).
Digital listeners (aged 50 to 69 years) of Bauer's radio stations and their biggest podcasts (including Confessions with Simon Mayo) will be targeted in a new and imaginative way. Using the 'Say It Now' feature, all they will need to say to their smart speaker is 'launch organ donation' and a link to the registration form will be sent directly to their phone!
As smart speaker listenership for adults 50+ is 46% and Bauer will ensure they are served 100% of the ads, this is both an effective and an innovative new channel for us, which simplifies the act of opting in.
Social Media Campaign
Adverts will also run across Facebook, Instagram and the Nextdoor app in high priority regions (North West, London, Midlands and Wales) where a lower proportion of the public have confirmed their decision to be an organ donor.
Timings
Activity will run across the above channels from 10 February to 31 March 2025. In Wales, activity to support will also include paid search, to ensure people searching for organ donation will see it as the top search result (this already happens in England), and local marketing and comms activity delivered by a Wales-based agency.
Living Donation:
Join us for the very first Living Donation Week.
In honour of World Kidney Day, we're celebrating the remarkable contributions of over 2000 individuals who have donated as living kidney donors via the UK Living Kidney Sharing Scheme.
What will happen during the campaign?
Throughout the week you'll hear from patients sharing their personal journeys along with experts explaining how living donation works, recognising the donors, recipients and dedicated teams that make it possible.
Join us in spreading awareness by sharing social media assets, patient stories and more!
For your information regarding Xenotransplantation (PDF 151KB)
Update from the OTDT Professional Development Team: Medical Education Update
Diagnosis of Death using Neurological Criteria 2025 update is launched
The Academy of Medical Royal Colleges (AoMRC) updated the Code of Practice for the Diagnosis and Confirmation of Death was launched on 1 January 2025. ICM colleagues, including all CLODs have been responding by working hard to establish and embed these changes, to maintain confidence in testing for a diagnosis of death in cases wherever this is possible. Whilst the diagnosis of death is independent of donation, with consent and authorisation known to be higher for donation in these patients, maintaining rates of testing and confidence in the process will be an important part in supporting a patient’s desire to donate. Early indicators are that this has been a successful launch and an opportunity to focus and coalesce around the practice of the new code.
The FICM website offers further information and resources of the new code:
Diagnosing Death using Neurological Criteria | The Faculty of Intensive Care Medicine
New Paediatric Line up:


As we bid farewell to Dr Reinout Mildner and Angie Scales as clinical leads for Paediatric and Neonatal Organ and Tissue Donation and Transplantation, we welcome Dr Omer Aziz and Sarah Plant in their respective new roles as National CLOD and Lead Nurse.
The National Deceased Donation Course scores 10/10!
At our latest course delivery in Cardiff, we facilitated learning for more ICM trainees in the principles and practices of donation.
Increasingly now trainees are part of the overseas CESR programme and we were delighted to receive really positive individualised praise from one such candidate who wrote:
"My sincere thanks and appreciation to all of you and everyone on the course faculty and organisers for the excellent organisation, teaching and discussions on the course. This has turned out to be one of the best courses I've attended over my (14 year) career" finishing that it gave some "very valuable insights and structure in the area of organ donation, legal and ethical considerations and the nuances of patient and family discussions and breaking bad news and EoLC"
Update from the OTDT Statistics & Clinical Research Team
Risk Communication Tools
2021 saw the successful deployment of the NHSBT Risk Communication Tools.
The NHSBT Risk Communication Tools are an online personalised calculator that can help clinicians communicate risk and benefit about transplantation to patients and can help patients more easily understand the numbers and statistics presented to them in clinic. It helps visualise possible outcomes for patients from the point of listing or point of transplant for deceased donor transplantation.
The statistical models for all 5 Risk Communication Tools have been updated and the Risk Communication Tools will reflect the changes made 3 March 2025.
The tool can be accessed via the tools, policies and guidance page on the ODT Clinical website, via the benefits and risks of a lung transplant page on the Patient Information Tools website, or directly here.
Some of you may recall that while the development of the statistical models of the Lung and Kidney Risk Communication Tools was undertaken by the NHS Blood and Transplant Statistics and Clinical Research team, design was based on advice from the Winton Centre for Risk & Evidence Communication at the University of Cambridge. The Winton Centre for Risk and Evidence Communication therefore also hosted tools for Lung and Kidneys patients regarding the Communication and risk and benefits around transplantation. As the statistical models have now been updated and the Risk Communication Tools will reflect theses changes, from 3 March 2025, the Winton Centre Tools will no longer be accessible.
The NHSBT Statistics team are working on further improvements to the Risk Communication Tools for users this year and more updates will follow.
We hope the Risk Communication Tools continue to inform discussions in the difficult decisions that often arise for patients and clinicians during their journey in transplantation.
Update on behalf of the National Liver Offering Scheme Review Survey
We're inviting patients, and family members of patients, who have received a liver transplant, are on the waiting list, or may need a liver transplant in the future to participate in an online survey about the National Liver Offering Scheme (NLOS), which is currently under review. Donor families and members of the public are also being invited to participate in the survey. This survey aims to gather patient experiences and insights to help improve the liver transplant allocation process. By participating, your patients can have a direct impact on the future of liver transplant services in the UK.
More information is available on the British Liver Trust Website and includes a link to the survey.
Please share this opportunity widely.
Thank you.
